NIPAH VIRUS
Why in news?
Kerala will intensify the disease surveillance activities and maintain vigil against Nipah across the State as Nipah virus antibodies have been detected in bats in Wayanad as well in Indian Council of Medical Research’s bat surveillance studies, Health Minister Veena George said on October 25.
About Nipah Virus
- Nipah virus (NiV) was first discovered in 1999 following an outbreak of disease in pigs and people in Malaysia and Singapore.
- The virus has been shown to spread from person-to-person in these outbreaks, raising concerns about the potential for NiV to cause a global pandemic.
- NiV is a member of the family Paramyxoviridae, genus Henipavirus.
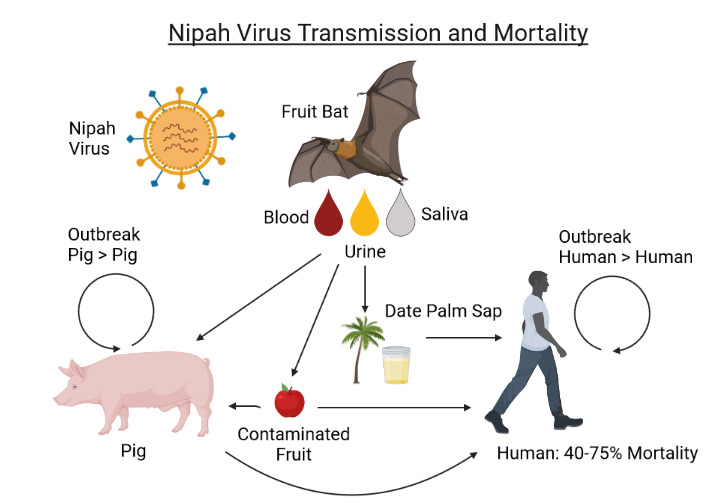
- It is a zoonotic virus, meaning that it initially spreads between animals and people.
- The animal host reservoir for NiV is the fruit bat (genus Pteropus), also known as the flying fox.
- Given that NiV is genetically related to Hendra virus, another henipavirus known to be carried by bats, bat species were quickly singled out for investigation and flying foxes were subsequently identified as the reservoir.
- Infected fruit bats can spread the disease to people or other animals, such as pigs.
- People can become infected if they have close contact with an infected animal or its body fluids (such as saliva or urine)—this initial spread from an animal to a person is known as a spillover event.
- Once it spreads to people, person-to-person spread of NiV can also occur.
- The symptoms of NiV infection range from mild to severe, with death occurring in 40%–70% of those infected in documented outbreaks between 1998 and 2018.
What are signs and symptoms?
- It usually presents as fever and swelling of the brain called encephalitis.
- Headache.
- Breathing difficulties.
- Cough and sore throat.
- Diarrhoea.
- Vomiting.
- Muscle pain and severe weakness.
- In extreme cases, disorientation and seizures
How is Nipah transmitted?
- The first outbreaks of the Nipah virus among humans was reported from Malaysia (1998) and Singapore (1999).
- The virus takes its name from the village in Malaysia where the person in whom the virus was first isolated died of the disease.
- The transmission from animals happens mainly through consumption of contaminated food. According to the CDC, transmission can happen due to “consumption of raw date palm sap or fruit that has been contaminated with saliva or urine from infected bats.
- Some cases of NiV [Nipah] infection have also been reported among people who climb trees where bats often roost.”
- The animal host reservoir for this virus is known to be the fruit bat, commonly known as flying fox.
- Fruit bats are known to transmit this virus to other animals like pigs, and also dogs, cats, goats, horses and sheep.
- Humans get infected mainly through direct contact with these animals, or through consumption of food contaminated by saliva or urine of these infected animals.
- But human-to-human transmission is also considered possible.
- The CD says “person-to-person spread of NiV is regularly reported in Bangladesh and India. This is most commonly seen in the families and caregivers of NiV-infected patients, and in healthcare settings.”
- Since it was first identified in 1998-99, there have been multiple outbreaks of the Nipah virus, all of them in South and Southeast Asian nations. In Bangladesh, there have been at least 10 outbreaks since 2001.
- In India, West Bengal had seen an outbreak in 2001 and 2007, while Kerala had reported several cases in 2018, and isolated cases in 2019 and 2021.
- The Nipah virus is known to spread far more slowly than SARS-CoV-2. However, it is its ability to kill that is the biggest concern.
How is nipah virus diagnosed?
- A real-time polymerase chain reaction (RT-PCR) test can confirm nipah virus through nasal or throat swabs, cerebrospinal fluid (CSF), urine and blood samples.
- Doctors can diagnose the infection in its later stages or after recovery by testing your blood for certain antibodies through the ELISA test.
How is nipah virus treated?
- There are no antivirals and there is only symptomatic management.
- Options are drinking water, resting, using medication to control nausea or vomitting, inhalers and nebulisers for breathing and anti-seizure medication in extreme cases are the present options.
- Researchers are studying using monoclonal antibody treatment.
- There’s no vaccine or medications to cure nipah virus.